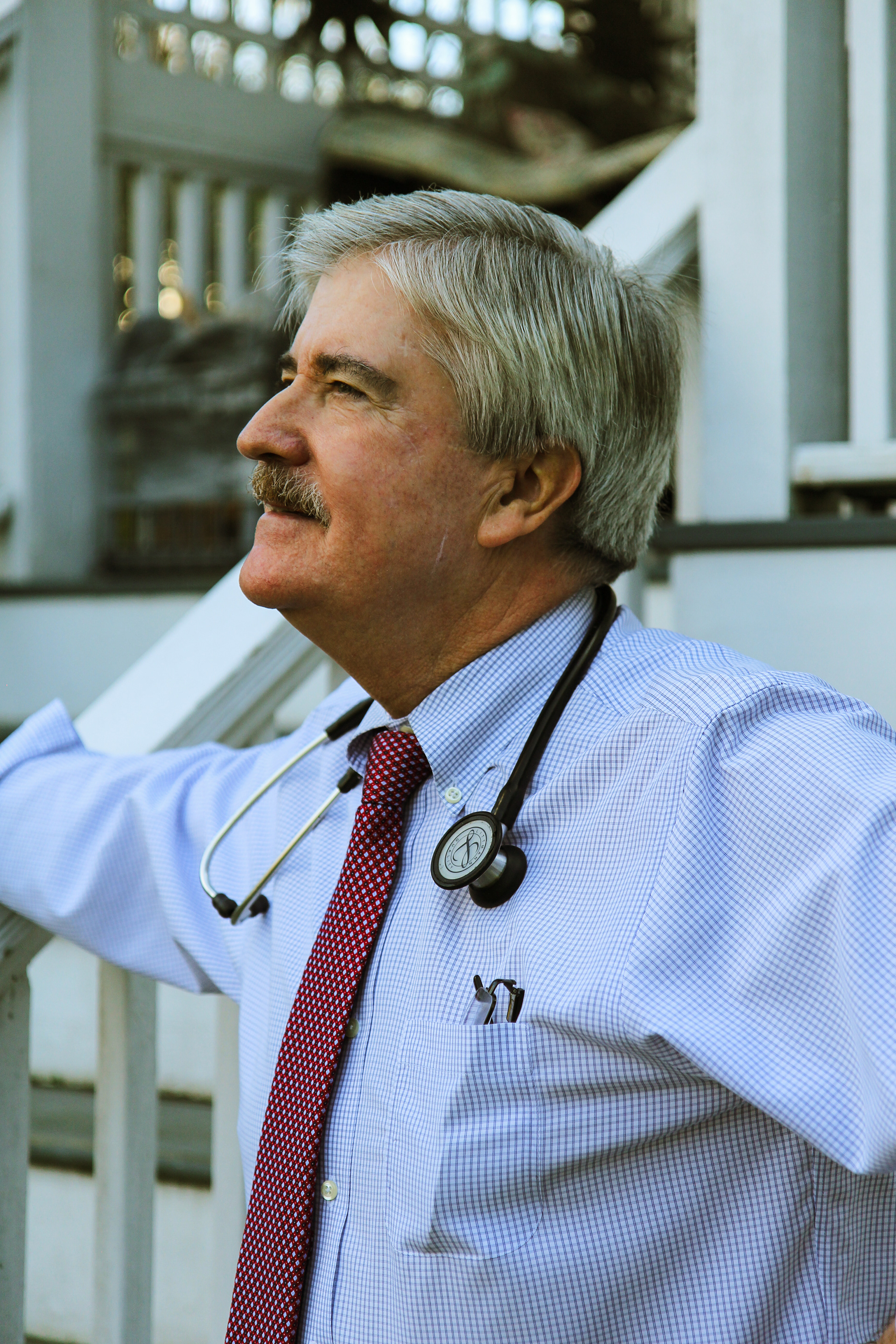
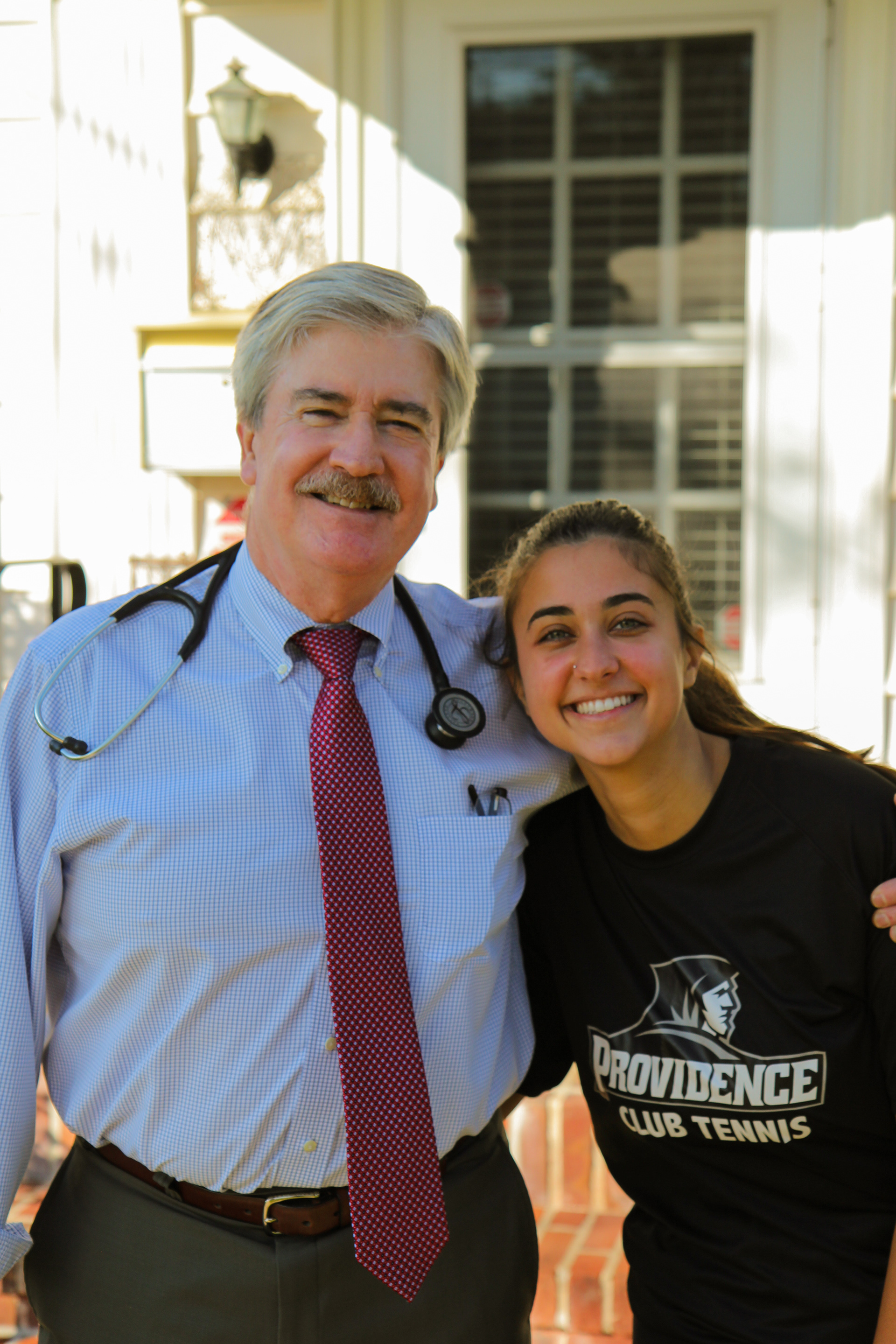
Dr. Alan Morelli
65, Pediatrician Navigating COVID-19
As a pediatrician in Stamford, Dr. Morelli has become well-acquainted with the collective uneasiness felt by our community these last 9 months.
During our conversation this Fall, Dr. Morelli shared stories from the beginning of his career, sharply contrasting them against the stressful effects of the pandemic on private medical practices today.
We discussed the changes he has observed in his patients and the city during a time of hysteria, and how testing positive for COVID-19 has impacted life for him personally.
Photographed and Interviewed by Alexandra Cali
September 30, 2020
Getting To Know Alan
Alexandra Cali: Let’s get started! Can you introduce yourself?
Alan Morelli: My name is Alan Morelli and I’m 65 years old.
AC: How long have you lived in Stamford?
AM: I moved to Stamford in 1985, and that’s around the time that I began practicing as a pediatrician. I did my residency from 1982 to 1985 in New Haven at Yale. After that, I had to give four years to the U.S. Public Health Service because they funded my scholarship for medical school. I was very lucky to get a position in Stamford through them.
AC: Were you assigned to one of the major hospitals in the area?
AM: I actually started a very small clinic all by myself on Selleck Street with the help of the Southfield Community Organization. They petitioned the federal government to have a doctor come there, because that side of Interstate 95 used to be pretty down and out. They didn’t have access to great healthcare. 35 years ago, there was a lot of crime and poverty in that area of the city, so I felt a great sense of responsibility stepping into the community.
AC: When did the office end up officially opening?
AM: We started seeing patients on November 1st, 1985. I loved what I was doing, but I was paid a very meager salary. $28,000 a year to be a doctor. So I had to work three other jobs to make ends meet.
AC: What did you do?
I would moonlight for a small practice at night. I was on call for them from Friday evening until Monday morning. I was also the physician for the Stamford Public School System. If a child enrolled at one of the public schools didn’t have a primary doctor, they would be assigned to me. On top of that, I was also the Stamford Well Baby doctor. That was a program for families on Medicaid, and they could bring their babies in for immunizations. I did all of that for four years.
AC: It sounds like you’ve had the opportunity to work with families from all different walks of life. What was that like, seeing how the economic inequalities in Stamford manifest when it comes to healthcare?
AM: It was interesting, starting my career here. You have wealthy families from these neighboring communities like Greenwich who are very lucky, very blessed to be able to afford whatever it is their children need. And then you see families who are in more desperate situations, with a lot of these kids making up the medically underserved population of inner city Stamford.
"A lot of the private practices in Connecticut don’t accept Medicaid because of the lower reimbursement rates, and it leaves these parents in a precarious position. I was able to transition a lot of the kids I met through the Stamford Public Schools System or the Well Baby program into my clinic. But the disparity in care options was and still is very apparent."
Changes In The Medical Field As Pandemic Hits
AC: Speaking of your current practice, I wanted to know how you guys have been faring since the beginning of the pandemic?
AM: It’s been hard. On days that are slow, my partners and I are obviously making less. But we still have to find a way to pay our staff who are full-time. And we need our full-time staff, they help keep everything moving forward and running smoothly. Unpredictable times are hard for private practices.
AC: Was there a noticeable uptick in patients coming in during the pandemic, and if so was it overwhelming for you?
AM: Funny enough, at the beginning of the pandemic the number of patients coming in really went down. Back in March, people were taking the stay at home orders pretty seriously. Appointments went down by about 50 percent I would say.
AC: What are things like right now for you?
AM: Right now, we have a lot more people coming in. Because we're just wrapping up the summer and going back to school, all these young kids are mingling. A lot of people relaxed their outlook on social distancing because there were fewer cases during the summer. Now we have to get ready for a second wave, which I can't say I'm looking forward to.
AC: Do you feel like your patients understand the gravity of the situation even though they are so little?
AM: Oh, definitely. I can't tell you how many little kids are terrified to take off their masks. I'll ask them to move it down past their chin during an appointment, and they'll look off to their parents in fear. They completely understand how deadly the virus is. If you think your generation is anxious, you should look at the kids who are growing up during all of this.
AC: While we're talking about anxiety, do you see a lot of frightened or misinformed parents coming in to ask questions?
AM: Yes. We've had some parents come in and say that they are terrified to send their kids back to school. Other parents have come in trying to get a better understanding of what symptoms look like and how the virus is spread. The media has done a poor job of circulating helpful information from actual health professionals. The most I've seen it do is stoke a lot of fear and confusion.
"I think one of the biggest things that brings comfort to my patients is talking about my experience with testing positive. I'm still here and I'm okay. When they meet someone who has gone through it, it puts them much more at ease."
Testing Positive For COVID-19
AC: I know you tested positive back in March. During that time, was it difficult to get a test?
AM: It was definitely harder to get one than it is now, even as someone working in healthcare. In March, the U.S. had very strict guidelines around who could go in for testing because of the high demand. They didn't want to overwhelm the labs, and rapid tests were not a thing yet. They had to send my culture off to a lab in California, and my biggest fear was that I would get I would receive a false negative due to the bacteria dying during travel time.
AC: What were your symptoms like?
AM: The first few days I had a fever, muscle aches, and coughing. At 65, I'm technically part of the age group that is most at risk. Thankfully, I had very mild symptoms. When I was first coming down with COVID, I was still riding my bike several miles each day and keeping up with my active lifestyle. I was very lucky that it didn't impact my lungs the way it does others. I've learned that these are the types of stories people really like to hear about. It gives them hope.AC: How did the people in your life react to you testing positive?
AM: Interestingly enough, some of the people at my practice seemed upset. I think it was just overwhelming to hear, because now people wanted to get tests for themselves. It was also challenging because that meant I wouldn't be able to see patients while quarantining. Thankfully, my patients and peers were fine because I wear so much gear during the work day. [My wife and daughter] even tested negative! AC: Reflecting on that initially alarming period of time, how do you feel now?
AM: I feel like I'm Superman. I had COVID and thankfully I didn't have it bad. Even though I'm seeing many patients each day that have symptoms and could potentially be positive, I know that I can't stop doing what I'm doing even though it's a little frightening. Because I have the antibodies, I know that I'm in the best position possible considering my line of work.Final Thoughts
AC: How do you manage the stress of being in a position where you are in such high demand?
AM: I'm very lucky that I was never called upon to work in one of the major hospitals. It almost got to that point during March, and that was scary to me. I try and take it day by day. Telling my story to patients and their families brings them peace, and in turn makes me feel better. Things at our office are ramping up, but it's the people on the front line in ERs that I worry about and have immense respect for.
AC: Would you say there has been anything in your career that compares to this pandemic?
AM: When I was a 3rd year medical student in 1980, there were these gay men dying from an illness that no one understood. We didn't know how to treat it, because it wasn't an airborne disease. Of course, we know now that HIV is a sexually transmitted disease. All of that hysteria, the race to understand and address an illness, the overwhelming number of people dying: the AIDs crisis is the only thing I can really compare this pandemic to.
AC: What advice would you give to medical students who are entering the workforce under unprecedented circumstances?
AM: I would tell them that it's going to be okay. I would understand if many of them feel lost or overwhelmed. Hospitals have great counseling services in place to support their doctors, and now more than ever these young people should rely on that. Know that they have a community within their workplace to lean on when things get tough. And I would remind them to not forget about themselves. Sometimes as doctors, we forget to check in and take care of our own needs.
AC: That is beautiful advice. Thank you so much for taking the time to chat with me.
AM: Oh, it's my pleasure.